Interview With Dr. Joanne KurtzbergLearn more about the history and origins of cord blood banking from an exclusive interview with CBA President, Dr. Joanne Kurtzberg. Q: How did the idea of using cord blood as a source of stem cells come about? A: In the mid-1980s, Dr. Hal Broxmeyer was conducting research on hematopoietic stem and progenitor cells. In his work, he found that cord blood contained blood stem and progenitor cells that were younger and more potent than those from bone marrow. He showed that cord blood cells were enriched, cell for cell, for myeloerythroid colony forming units and that cord blood cells could rescue more generations of mice in serial transplantation. This led Hal to hypothesize that cord blood could substitute for bone marrow as a donor for bone marrow transplantation. Ultimately this was tested in 1988 in a matched sibling cord blood transplant performed by Dr. Eliane Gluckman in Paris in a 5-year-old boy with Fanconi Anemia. Q: How did that first cord blood transplant in 1988 influence you? A: I was a pediatric hematology oncology physician caring for the recipient of the first cord blood transplant. The boy was diagnosed with Fanconi Anemia at 2 years of age and developed full marrow aplasia when he was 4 years old. Around this time, his mother happened to become pregnant with another child. We arranged to have Dr. Arleen Auerbach test an amniotic fluid sample to determine if the fetus was affected with Fanconi Anemia. Arleen returned great news, the fetus was healthy and was an HLA match for her brother. Arleen, Hal, and other investigators from Memorial Sloan Kettering Cancer Cerubnter (MSKCC) were working together to test whether cord blood could be a good source of hematopoietic stem cells and when the information about this family was learned, they approached me and my husband (also a Peds Heme/Onc MD) to ask if this family would be willing to allow their son to receive a cord blood transplant. The family said yes, and many troops were mobilized. Dr. Gordon Douglas, an OB from New York City, attended the delivery in Salisbury, North Carolina, and collected the cord blood. The cord blood was shipped to Hal Broxmeyer who froze it in his lab at MSKCC. After the baby was ~6 months old, the family travelled to France where Dr. Gluckman performed the transplant. Hal and Scott Cooper transported the cryopreserved cord blood unit in a dry shipper on a commercial airliner in a passenger seat a few days before the transplant. Fortunately everything went well, the child engrafted and had no complications from the transplant. That was in 1988. Today, 36 years later, he’s alive and well and fully engrafted with his baby sister’s cord blood. I started the Pediatric Blood and Marrow Transplant Program at Duke in 1990. From the beginning, I focused the program on performing transplants from cord blood, especially for patients lacking matched donors in their family or through the NMDP. I also was inspired to start a public cord blood bank at Duke, the Carolinas Cord Blood Bank, which obtained a BLA from the FDA in 2012 and which continues to operate to this day. 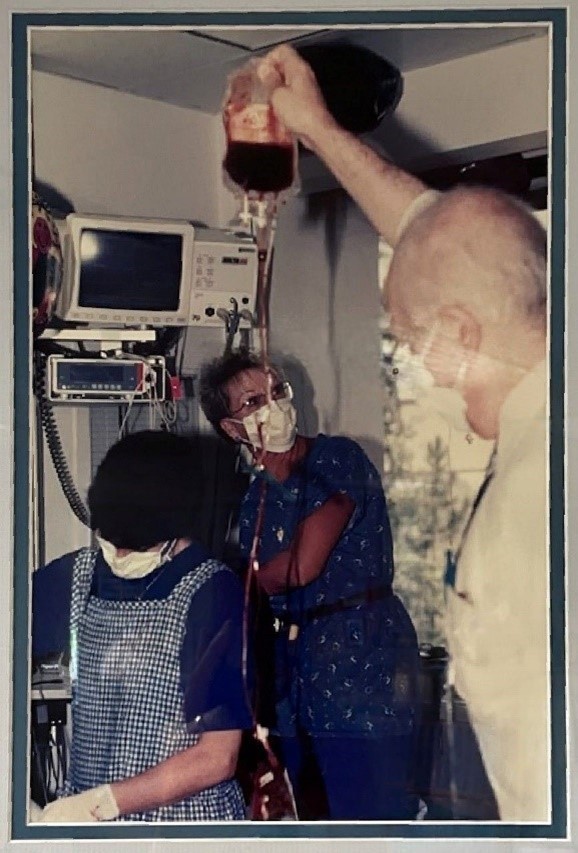 Q: What led to collecting, cryopreserving, storing, thawing, and infusing cord blood for transplantation and the creation of the first public cord blood bank by Dr. Pablo Rubinstein? A: Dr. Rubinstein worked with Dr. Broxmeyer in the early days of related cord blood transplant and created and established the first procedures for collecting, processing, cryopreserving, and thawing cord blood units for clinical use. He established the first public cord blood bank in the USA at the New York Blood Center in 1991.
*The image to the right features Dr. Joanne Kurtzberg and Dr. Pablo Rubinstein performing the first unrelated cord blood transplant in 1993.
Q: Describe your experience when performing the first unrelated cord blood transplant in 1993.
A: After we established the pediatric transplant program at Duke, we performed a few related cord blood transplants between 1991-1993. In those days, the cord blood community was small and we all knew and interacted with each other. A few other transplanters, including Dr. John Wagner at the University of Minnesota, had performed related cord blood transplants and observed that there was a lower incidence of acute and chronic graft versus host disease when cord blood donors were used as compared to bone marrow donors. That led to the idea that unrelated donor cord blood could be used as a donor source and also that full HLA matching might not be necessary. Pablo approached me to ask if we would be willing to perform an unrelated donor cord blood transplant at Duke using a unit from his bank and I said yes. We were caring for a 4-year-old boy with refractory T-cell ALL in relapse who did not have a fully matched related or unrelated donor. We identified a cord blood donor in Pablo’s bank and performed the transplant. Pablo came to Duke for the transplant, teaching us how to thaw and wash the unit in dextran and albumin. He attended the infusion as well. Q: What is your favorite story to share about Dr. Hal Broxmeyer?
A: There are many stories about Hal, who was a brilliant scientist, wonderful mentor, and compassionate and caring individual. One of the things I used to tease Hal about was that he called thawing of the cord blood unit, “defrosting” the cells. While he wasn’t incorrect, I thought thawing was a better way to describe the process. He continued to use the term ‘defrosting’ for his entire career.
Q: Do you have another story or experience about the early years of cord blood banking you want to share?
A: In the early years of our bank’s operations, we had a day when our regular courier was out sick. We utilized a courier service to pick up fresh units collected at one of our collection sites. The units were never delivered and when we checked with the courier, they produced a forged document stating that they delivered the units. We searched for the units for the next several days but never found them. A week later, we got a call from the courier service saying that the units had been located. It turned out that the courier had stopped at a fast-food restaurant for lunch and parked his car in the parking lot of the restaurant. The courier was behind on car payments and his car was repossessed by a collection company while he was eating. When he came out, the car was gone with the cord blood units inside. Needless to say, we couldn’t save the cord blood units. This taught us a lot about chain of custody, tracking of shipments, and, as the FDA says, ‘being in control of our processes.’
|
